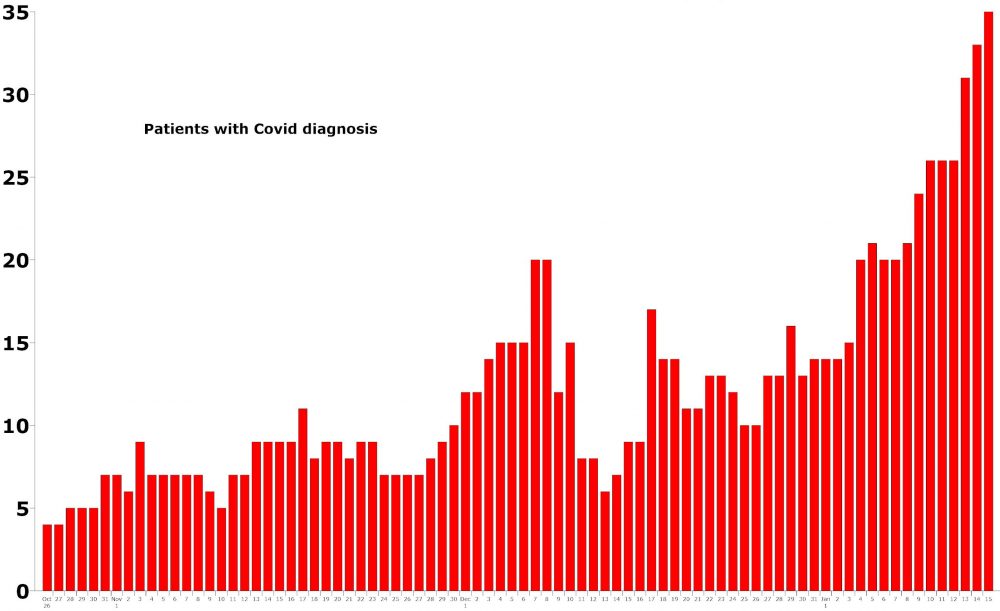
As Flagler County’s Covid-related, confirmed death toll reached 53 today, with the new year’s three deaths occurring between Jan. 7 and 8, AdventHealth Palm Coast’s census of patients hospitalized on a primary diagnosis of C ovid-19 broke a record for the sixth time since Jan. 1, reaching 35, a far larger number than the hospital contended with at any point in the pandemic.
The crush of hospitalization is a consequence of Flagler County’s post-holiday surge of confirmed new cases of coronavirus , a surge that has broken weekly case load records for the past four successive weeks, and appears poised to break the record again this week: 348 cases were confirmed in the past six days, with Saturday’s numbers yet unreported. Last week’s record was 398 cases. Almost a third of the More than a quarter of
Flagler County has confirmed 1,582 cases in the past five weeks alone: a third of all cases since the pandemic began in February.
During the first wave in March and April, when weekly case loads were in the mid-teens and never exceeded 61 for a single week, AdventHealth Palm Coast had put up a tent outside its emergency room, had prepared for ICU overflow, and had arranged with Palm Coast government to use the Palm Coast Community Center for some patients if the hospital itself was overrun. Numerous procedures and all elective surgeries were suspended, and numerous other restrictions instituted.
Last week, the hospital’s Central Florida division, which includes AdventHealth Palm Coast, placed its hospitals on Red Status, again instituting limits on elective surgeries and outpatient procedures. But despite the much higher number of patients, the tent has not gone up. There are no plans to tap into extra space at the Community Center. While the staff has been overtaxed by the length of the pandemic and the ongoing surge, its resilience has endured.
“Despite all the wear and tear that this virus has inflicted, worldwide, our staff has held up remarkably well, and that’s from great support in the community,” said Dr. Paul Mucciolo, AdventHealth Palm Coast’s ER medical director until last year, and the Chief of Staff since.
In a wide-ranging interview this morning about the hospital in the midst of this latest surge, Mucciolo discussed hospital supplies–no issues there, and plenty of ventilators–its capacity to handle the load more efficiently than in the spring, and the vaccine’s recent effects on morale. He explained the criteria for hospitalizations, the difference between treatments and protocols in the ongoing wave compared with the early months of the pandemic, when responses were less efficient and knowledge about the disease far more scant, and who gets transferred out with a Covid diagnosis and why. But he also discussed the ongoing problem of getting reluctant people who are experiencing serious medical episodes to the hospital, whether it’s heart attacks, strokes or other severe issues, because there remains a segment of the population that fears going there, again because of Covid.
The fear is misplaced, the reluctance life-threatening.
“I hate to see people have a debilitation that could be lifelong because of misinformation, some of the fear and uncertainty and the doubt that spread in some of the media, because they don’t look at things objectively. If you need to go to the hospital, you’ve got to come in. That’s where it sort of boils down to,” Mucciolo said.
Most essentially for residents to know: the hospital’s patient load is up, and not just because of Covid. But its ability to care for patients is not compromised because of the higher numbers.
“Because we’re in the southeast, we have the snowbirds, so we have a lot of people with other disease unrelated to Covid that are coming in as well, so that has put an extra burden on the system,” the doctor said. But the hospital and the hospital foundation, its non-profit arm, have compensated with streams of supplies and additional staff.
What does it take for a person to be hospitalized? “That is a bit of a complicated question,” Mucciolo said. “The primary reason we hospitalize them is respiratory compromise. It’s usually the people with the GI symptoms, the vomiting and the diarrhea. They usually do well with aggressive rehydration and medication therapy, and go home. The people with upper respiratory symptoms, the loss of taste and smell and generalized malaise, just aching, not feeling well, they generally do fine. But the problem is the respiratory compromise. That’s why when people say, oh, it’s just the flu, I’ve heard that: it’s not the flu. The flu does not affect your lungs like Covid does. That’s the primary reason that people are hospitalized.”
The 35 people in the hospital today are spread between ICU beds and other beds. “I see the hospitalists on a daily basis, and the intensivists on a daily basis,” Mucciolo said. “There are times when we’ll push our limit for the [ICU] unit. But I don’t think we’ve gone beyond it. No one has told me that, that I’ve talked to, none of the physician staff have told me that. We do have some of the Covid patients, just like other patients [who] come in for say, a community acquired bacterial pneumonia or congestive heart failure. They require ventilatory support with what we call BiPAP, which is a more sophisticated version of the C-pap machine people wear at night that you see advertised on TV for snoring. What it does is gives them respiratory support short of having a tube in their throat, going on a ventilator. We can manage those patients and we have regularly for years, before Covid, in the preventative care unit or the step-down unit, and they do well.”
The step-down unit, also called progressive care, is a step below intensive care. The hospital opened a $15 million addition in 2016, doubling its capacity of progressive care beds to 32. “The staffing is adequate, and importantly, the entire hospital staff are well trained and well geared to take care of the Covid patients from the one who has the loss of say, smell, to someone who is in respiratory distress,” Mucciolo said.

Not all Covid cases come through the ER. Some are diagnosed in the community, and are offered immunotherapy at home. The patients are selected carefully, and are only those who are obviously not in need of hospitalization. The goal is to decrease the risk of bad outcomes for patients with co-morbidities like high blood pressure, diabetes, obesity and the like: they are at far higher risk of developing complications from Covid. Mucciolo did not have exact numbers of the number of patients cared for that way, but he said “the adverse reaction rate is less than a single digit percent.”
As it did in earlier waves, AdventHealth Palm Coast continues to transfer out some patients with Covid-19. “We do transfer some patients out who require ECMO therapy,” that is, extracorporeal membrane oxygenation: the ECMO machine is a life-support system that replaces the functions of the heart and the lungs. ECMO had begun as a way to ventilate newborns with underdeveloped lungs. It has been found to be an effective life-saving treatment for some severely affected Covid-19 patients. AdventHealth Palm Coast doesn’t have that capability locally.
“It’s like dialysis for your lung,” Mucciolo said. “We do transfer some patients out for that, and we’ve had remarkable success rates with it. I don’t want to breach anyone’s confidentiality but some of it has been on Facebook, some of the patients that we had at Palm Coast, transferred to Orlando, were treated there aggressively with the ECMO therapy for a while, and then discharged, and did well. They survived, where normally they would not have.” Mucciolo was referring to Dr. Anthony Tucker, the well-known Palm Coast physician who wrote about his treatment on Facebook–what turned into a two-month hospitalization and ordeal that had him grazing the edges of life before his discharge on Dec. 18.
The significant difference between last spring and now is the trove of experience and knowledge physicians and staff have accumulated and shared across hospitals, including AdventHealth’s own team of scientists and researchers, all of it combining to reduce some of the guesswork in the battle against Covid make the battle less like “War of the Worlds” and increasingly more like a difficult but conventional struggle against a virulent but not indomitable pandemic. “Health care has adapted remarkably well to this,” Mucciolo said.
That’s what made last spring’s hectic and ominous preparations superfluous this time around. “They’re not necessary, and the reasons are not because of the volume of patients, but because of our efficiency,” Mucciolo said. “We’re much better at identifying: the test is much faster, it’s much more reliable, and the test that we have is the PCR, which is the gold standard, but it tests for influenza A, influenza B, Covid-19 as well as RSV,” the acronym for respiratory syncytial virus, which causes common-cold-like symptoms. “So it helps us sort out co-infections or other infections that can give you similar symptoms.”
At the same time, the so-called Case Mix Index, a key indicator of the complexity of patients’ medical conditions, has “definitely” risen. “This has added another layer to the cake, so to speak. Covid-19 has,” he said, one reason being that people have been waiting too long to come to the hospital after developing serious medical issues.
“What I’d like to do is encourage people to please come in if they come in if they have stroke symptoms, please come in if you’re having chest pains, please come in if you have a high fever and pneumonia symptoms, and you’re short of breath,” the doctor said. “We still have a reluctance of people to do this, and we’re missing the window on being able to deliver optimal outcomes. It’s not just in AdventHealth Palm Coast. It’s nationwide. This is on all the emergency medicine literature. So we have to get it out to people, the Do’s and the Don’ts. Don’t come in because you want a screening test. If you’re not sick, there are community alternatives that are faster and easier, because that will bog us down and we don’t have the testing capability to handle that. Our capabilities are for people who are symptomatic and ill. I can’t emphasize enough the importance of coming in and coming in early. I know that it’s a hard thing to do, but I have to emphasize to people: forget the Covid scare if you have stroke symptoms, because we have every precaution in place for our patients. It’s like I talk to a friend of mine who is a physician in the military. He said it’s like being on an aircraft carrier in a conflict. It’s the safest place to be, because everyone knows what to do, they know the protocol, they know the drill. It’s the same thing with the hospital. People say, well, I was afraid to come in because of Covid. But we missed the time window to treat their stroke. We missed the time window for their heart attack.”
The vaccine has not quite been a game-changer–yet: it cannot be, until a far larger portion of the population is inoculated. But it’s had its effect in matters of morale among staff, since it does provide a level of protection that eliminates deep anxieties about exposure to the disease. Still, Mucciolo said, “it’s not a substitute for a mask, washing your hands, touching your face, maintaining social distancing. But it’s an extra layer of protection, because we have to see how long the antibodies will last.” (And there’s a very small segment of the population, like Mucciolo himself, whose bodies don’t respond to vaccines.)
“At our facility, it’s been embraced, and enthusiastically everyone is following up with the vaccine because of the robust education protocols that the hospital has in place,” Mucciolo said.
The hospital has not been burdened by residents seeking the vaccine at the ER. “The primary misinformation is still about the testing, because they will look it up somewhere and get misinformation off the internet or from a friend or from somewhere, and they come in, ‘I want a test,’ and they have no symptoms whatsoever,” Mucciolo said. “The emergency department is not set up for that. We have to use our resources for the patients who really need it.”
For now, as AdventHealth’s hospitals are seeing record loads across the system since the beginning of the pandemic, the question is whether Flagler County has peaked. “I’ve got my fingers crossed and nobody has a crystal ball, but I think we’re about at it now, because it seems like it would start in the larger areas like Jacksonville, Orlando, Miami, the Tampa area, and then out in the west part of the state,” Mucciolo said, “and then kind of propagate out from there, which makes sense because they’re more congested. Those areas are I think coming down a little bit. We should be–hopefully–seeing the benefit of that over the next week or so.”





























B&B says
With all this going on I am shocked that the workers all around town are not wearing masks. One would think the Town would request anyone contracted to work in the community to wear a darn mask.
Set the example. Use you brain.
Give a darn.
Trump/Covid2020 says
New records highs of Covid cases and deaths?!?!?!?!?! Can’t be true. One of our “leaders” told me it would disappear this summer, we were rounding the curve and after the election it would disappear. Was my dear “leader” lying to me? Numbers sound rigged. Rudy Giuliani and his crack legal team should look it into this. I mean really…did the signatures of the people who died even match? Likely numbers cooked up by Obama, BLM and Antifa to make Trump look bad so leebrals be turnin us into Cuba.
Harvey Dingle says
Fortunately, Flagler County is getting more vaccines on Tuesday. FlaglerLive needs to provide a retraction of an article claiming no vaccines for 5 weeks. You got it wrong and caused panic. And than blamed DeSantis. You provide a disservice to the residents of Flagler County.
From a real news source.
Flagler County will likely get a new allotment of COVID-19 vaccines on Tuesday, Jan. 19, Florida Department of Health-Flagler Health Officer Bob Snyder said on Flagler Broadcasting’s “Free For All Friday” radio program Jan. 15. Officials do not yet know how many doses will be available.
FlaglerLive says
FlaglerLive reported Snyder’s comments a day before he made them on the radio, and the previous article you refer to still holds: Jonathan Lord was quoted as saying that Flagler’s Health Department would get “few if any” vaccines in the next five weeks. The department got none this week. It got none last week. It is getting a few next week. It has no idea how much. According to Jared Moskowitz, not even his agency knows what’s coming more than six days ahead of time, and what’s ahead is, as Lord said, in the range of “little.” Finally, you heard about this on WNZF, unquestionably a real news source, because it is a partner of FlaglerLive and relies on FlaglerLive for much of its news reporting, often lifted word for word from our articles–with our blessing and appreciation: we wouldn’t want them relying on more dubious sources, though they often fall for local government PR posing as news.
Skibum says
All of us owe a HUGE debt of gratitude to the many local health care workers and first responders who have been taking care of the COVID-19 patients in Flagler County for the better part of a year now. We can support them by practicing social distancing, wearing our masks when in public, and not putting ourselves in danger of contracting the virus by doing dumb things that we know are in violation of the well known medical guidelines that we all should be following at this point. I’m sure many of the health care workers get disheartened when they see people so cavalierly violate CDC protocols while these hospital workers are sometimes overwhelmed with patients that may not survive after being infected and hospitalized. Let’s help our health care workers and first responders by doing the right thing and lessen the burden they carry as they work to save lives.
Mark says
Even with a vaccine you will be required to wear a mask and social distance for years to come. The vaccine does not stop you from getting coronavirus , or from transmitting it to others. The vaccine only provides protection from getting symptoms. So even when you get the vaccine, WEAR A MASK AND STAY HOME!
Carol says
January 19 3:06 pm
I registered for text alert with county health department to receive updates on vaccine availability. A few minutes ago I received an alert that limited quantities of the vaccine were available and it gave me a website to contact. I immediately did so and got a Google page with multiple options for the health department…… I chose the county Health Department website and there was NO information about what to do with my recent text alert…What in heavens name is going on here.???
If the health department’s text alert system isn’t functioning……which apparently it isn’t….then this department is wasting our time and not serving the community.
We need answers and results.
Carol says
I forgot to add to my above post that I called the Health Department number and could not get through to anyone…… just a bizzillion references of who to call, including one to volunteer…….but no information re my text alert!