Last Updated: February 12, 5 p.m.
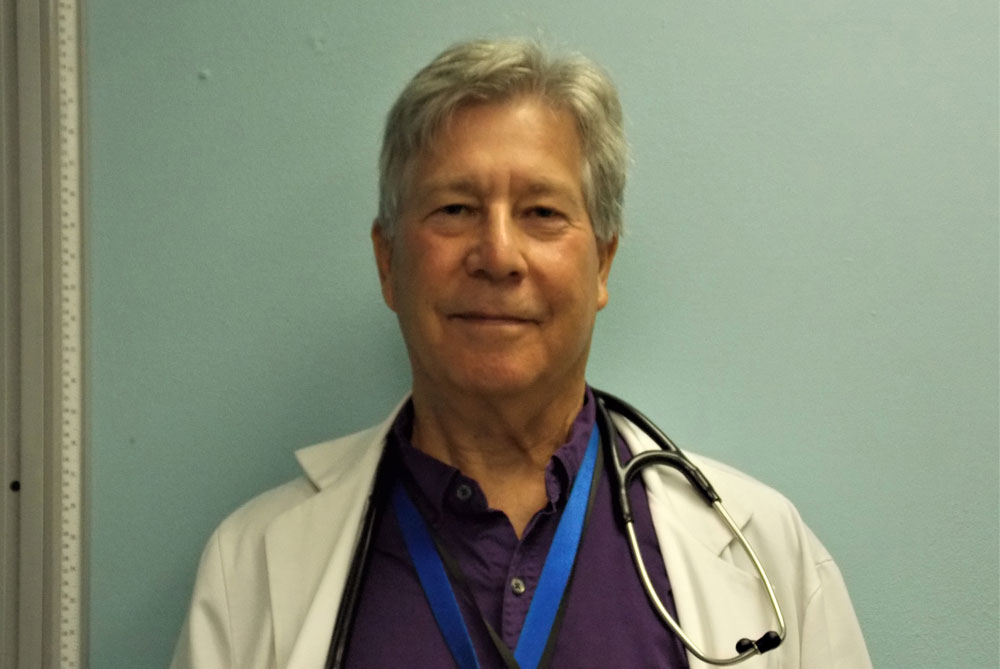
Here’s the fourth installment of FlaglerLive’s “Ask the Doctor” column by Dr. Stephen Bickel, the medical director at the Flagler and Volusia Counties Health Departments. Below are his answers almost two dozen new questions submitted in the past days, including a dozen quite specific questions about the coronavirus vaccine and other issues.
Dr. Bickel, featured almost weekly on WNZF’s Free For All Friday program since last March to update the community on the coronavirus pandemic and answer questions, will be doing so on a rolling basis here. The questions don’t have to be limited to the pandemic.
You are invited to submit your questions using the form below, or by email, or in the comment section below. The entire list of questions will be archived, indexed and linked to their answers on a separate page, here.
As Dr. Bickel describes it, “the “Ask the Doctor” column will be a semi-regular feature of FlaglerLive, the frequency of which will depend on the volume of questions we receive. The updated timestamp in red at the top of the page, will indicate when new question s have been answered.
Please feel free to ask any medical question you want, and I will do my best to answer it. In preparing my answer to your question, I may consult with some of my medical specialist colleagues or review the medical literature in order to come up with the best possible answer.
“Please limit your questions to general medical advice—I can’t give you specific medical advice since I don’t know your individual medical history. The emphasis of this column will be to provide information based on current scientific evidence while keeping speculation and politics to a minimum. If I don’t know something or the medical literature really doesn’t have much to say on a particular topic, I will tell you that.
“The fields of medicine and science in general are always advancing and we don’t have all the answers, but I will try to come up with something helpful for every question I receive, even our knowledge in an area is limited. At first a lot of the questions may be about Covid-19, but they don’t have to be, and any area of medicine is fair game for this column.”
The inaugural installment of the “Ask the Doctor” column, also about vaccines, is available here, the second installment is here, the third is here.
![]()
By Stephen R. Bickel, M.D.
Specific Medical or Safety Questions
I have three children (7, 5, and 3) that have spent the last 10 months at home. Our hope is that it is safe for them to attend public school in person again this coming fall. Given that all forms of the vaccine are not approved for anyone younger that 16, and won’t be by fall, how safe is it for young children to attend school in the fall? [Blake VandeBunte]
Returning our children to school is, and should be, one of society’s highest priorities. You, as a parent, have the difficult task of balancing the medical risks of school attendance with the social and scholastic benefits of attending school. Here are some thoughts that could help. Children tend to have milder Covid symptoms than adults and the risk of death is almost zero.
While it is unlikely that pediatric vaccination will be approved before next school year, many of the people they will be coming in contact with COULD be vaccinated by then: you parents, teachers, grandparents, parents of your kids’ friends, etc. Thus the vaccination roll-out will indirectly protect your kids from getting infected even before they can be vaccinated themselves.
Studies suggest that most Covid cases among school children and teachers are contracted outside of school. This underscores the importance of protecting your children after school through mask usage, social distancing, avoiding indoor exposure to groups, and handwashing.
Appropriate in-school protective measures are vitally important. You should be aware of the measures taken by your school, particularly regarding mask enforcement, distancing, and ventilation. Additional public health measures within the school, including testing, tracing, and quarantine, will help prevent and contain outbreaks.
In conclusion, I hope, and anticipate, that you will be able to safely send your kids back to school next fall or sooner (even now). In addition to all of the precautions you have been taking, I suggest you encourage everyone you know to receive vaccination as soon as it is offered for their age and occupation. And please continue to support your schools in their effort to do everything possible to make school safe for the students and the teachers. Parenting has never been easy, and the pandemic has made it even harder. Hopefully the balance between the risks and the benefits of school attendance will keep shifting in the right direction to make this decision easier for you.
This may fall into the Urban Myth category, but if there is any actual data on the subject, I’d be very interested to hear/read it, or read your comments. What effect might an autoimmune disorder have on an individual’s response to the Covid-19 virus? Is there any chance that following a protocol of avoiding certain substances enhances the body’s ability to respond? (One theory going around social media about ten years ago was that eschewing gluten helped mitigate the effects of chemotherapy, e.g.) This idle speculation was prompted by Tara Parker Pope’s article on the low percentage of coronavirus patients in China who wore glasses.
Although some of the more serious clinical manifestations of Covid-19 are thought to be due to dysregulation of the immune system triggered by the infection, I am not aware of any studies documenting that patients with autoimmune disorders have worse outcomes with Covid-19, but it would not surprise me if they did. Also, keep in mind that autoimmune disorders are a very heterogeneous group of conditions, so what applies to one condition may not apply to others. In addition, there is the factor of whether a patient is on immunosuppressive medication for their condition to consider, and that may have more of an effect than anything else. As a group, patients who are immunosuppressed are expected to have worse outcomes with Covid-19, but again that effect is highly variable.
Regarding whether certain substances (like nutritional supplements, vitamins, herbal preparations) improve the body’s ability to respond to SARS-CoV-2, many have been suggested–including vitamins C and D, thiamine, melatonin, zinc, and quercetin. The evidence is strongest for vitamin D, but still not conclusive.
Regarding whether eye protection helps prevent getting Covid-19, there is some evidence to support this, including a meta-analysis published last summer in the Lancet and linked below, which concluded that facial coverings such as masks, eye protection, and social distancing starting at 3 feet with an increasing effect at greater distances–were all effective to some degree:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31142-9/fulltext
Questions About the First or Second Dose and Eligibility for the Covid Vaccine:
How long before people with HIV can get vaccine?
Pretty soon! The next priority group (right after the over 65 age group) will include those with increased Covid risk due to their medical conditions, which includes persons living with HIV.
I’m 76, diagnosed with PBC and have had the first dose of Moderna vaccine thanks to the fine folks at Cattleman’s. Presuming I get the second dose and an antibody test shows strong antibodies, can I still get the virus? Or give it to my family who have not had the vaccine?
Although the Moderna vaccine provides excellent protection against getting Covid disease (symptomatic Covid), the degree to which it protects against asymptomatic Covid infection is still somewhat unknown, so it is theoretically possible for you to get an asymptomatic Covid infection after being vaccinated, in which case you could spread it to unvaccinated family members. You can significantly decrease the chances of this happening by practicing preventive measures such as masking, social distancing, etc.
Regarding testing for antibodies after vaccination, this practice is not recommended at this time except maybe in special circumstances such as individuals who are immunosuppressed. Since both the Moderna and Pfizer vaccines protected approximately 95% of individuals from getting even mild to moderate infections (and virtually 100% of severe infections), it is unlikely that antibody testing will add much clinically useful information except in immunosuppressed individuals.
My husband and I received our first shot as seniors on January 7. Will we be able to get our second shot ahead of new vaccine seniors or will we have to scramble to get ours.
The current policy is to set aside enough vaccine doses each week to make sure that all individuals who got first shots get their second shots on schedule–lately the Health Department has been receiving two shipments of vaccine a week, one for first shots and one for second shots.
My 16-year-old grandson has Ulcerative Colitis which is in remission with the use of Humira injections every 10 days. Can he get the vaccine?
Yes, he can get vaccinated, but only with the Pfizer vaccine, which is authorized for individuals 16 years of age and older, but not the Moderna vaccine, which is only authorized for individuals 18 years of age and older. The Humira injections will probably diminish to some degree his immune response to the vaccine, but it is still recommended that he receive it and neither the ulcerative colitis nor the Humira injections are contraindications to getting vaccinated, providing his medical condition is stable. I also recommend that you check with his medical provider (the one who is prescribing the Humira) to confirm that what I just wrote applies to his particular medical situation and also regarding the ideal timing of getting vaccinated in relation to when he gets his Humira injections.
As someone who is immune compromised, Addison’s disease, I know I may not produce as many antibodies after the COVID vaccine as most. Would an antibody test be useful in determining how robust my response is? Exactly what information can be gleaned from an antibody test? [Elizabeth Graf]
The short answer is we don’t really know if antibody testing post-vaccination is useful in situations like yours, where there is a possibility that your response to the vaccine may be suboptimal. Check with your healthcare provider about this, as it may be useful in your particular situation. There are various antibody tests out there, so if you do get antibody testing, make sure it measures antibodies to the spike protein, which is what the vaccines stimulate. Also, keep in mind that inducing antibody production to the spike protein is one very important way these vaccines work, but it is not the only way, as the vaccines also stimulate T cells and B cells.
And here’s what the CDC had to say about the Covid vaccines: “Persons with autoimmune conditions–No data are currently available on the safety and efficacy of mRNA COVID-19 vaccines in persons with autoimmune conditions, though these persons were eligible for enrollment in clinical trials. No imbalances were observed in the occurrence of symptoms consistent with autoimmune conditions or inflammatory disorders in clinical trial participants who received an mRNA COVID-19 vaccine compared to placebo. Persons with autoimmune conditions who have no contraindications to vaccination may receive an mRNA COVID-19 vaccine.”
I am 81. I have COPD,Neuropathy, and Thyroid Nodules. In your expert opinion am I a candidate for the vaccine? Thank you.
Yes, absolutely, you are a candidate for the vaccine, and none of the medical conditions you listed is a contraindication to getting vaccinated.
When will my adult disabled son be eligible to receive the vaccine?
In Florida right now, except for rare special exceptions, we’re just vaccinating health care workers and individuals over the age of 65. Once that group is vaccinated we’ll move onto the next group, which will include those with medical conditions putting them at increased risk for severe Covid outcomes (along with other groups that may be included). Depending on how that group is defined (to my knowledge this has not been fully worked out yet) your son may or may not qualify in this group. But as the spring rolls on there will be much more vaccine available and we hope to be able to vaccinate everyone who wants to be vaccinated by the summer if all goes well.
I don’t turn 65 until the end of February. Any information on when I’ll qualify for the vaccine? My husband and most of my friends are already able to get it and have received at least the first one.
You will qualify for the vaccine as soon as you turn 65–in just a few weeks.
I may have jumped the gun. I was online and scheduled an appointment for 1-29. My first dose was 1-5. That would make my four weeks 2-2. Is 1-29 too early? Should I keep or cancel my appointment?
Yes, it’s too early. The current recommendation is no earlier than 2 days before your scheduled 28 day interval between first and second doses, so you should reschedule, ideally to February 2. They should be able to reschedule this for you.
Questions About the Effects of the Vaccine:
I received the first dose of the Moderna vaccine on 1/8/21. About 10 seconds after the injection I felt a little “woozy”/dizzy which passed, however, I had an elevated heart rate for the rest of the evening. I’m wondering if it’s safe to get the second dose? I do not have a history of allergies. Thank you for your time.
Your immediate reaction to the shot sounds like a common, benign, reaction, the lay term for which is fainting. The technical term is “vaso-vagal” and it sometimes makes people pass out. It is nothing to worry about except to be aware that it could happen again. Just stay seated, bend over, or lie down if it happens. The elevated heart rate is not explained by a vaso-vagal reaction. If it was not extremely elevated (over 120 beats per minute) and you had no other symptoms (like chest pain, shortness of breath, or lightheadedness), it could be you were just a little anxious. If the heart rate was very fast, or was associated with other symptoms, please check with your doctor.
66-year-old male. Four days after second Pfizer vaccine experienced chills fever and body aches. Then nonstop diarrhea for five days. Staying hydrated pedialyte and water. Was told to take six – ten million Probiotic. On day two of that. Still cannot keep anything down. Any help would be thankful.
This would be a very unusual reaction to the vaccine–the symptoms are unusual and the four day delay is unusual. It is possible, but unlikely, that it’s due to the vaccine, but it sounds more like another medical condition or illness. I advise you to seek medical care for this if your symptoms have not resolved by now.
I am scheduled to get my first Covid vaccine this coming Tuesday. I having some pain on a tooth and think it might be an infection. I can’t see my Dentist until Thursday. if I get the injection on Tuesday and it’s determined I do have an infection on Thursday and need to take antibiotics will I be in any danger?
I anticipate no problem with interactions. I would get the vaccine then do what you need to do with the tooth. Good luck.
I am a breast cancer survivor. Stage 3. Diagnosed in 2015, finished all treatments in 2016. Presently on Femara until 2026. I am afraid this vaccine will make my cancer come back. Is it safe to get?
Here’s what the American Cancer Society had to say on this subject, which I agree with–this is from their website: “Although many expert medical groups are recommending that most patients with cancer or a history of cancer should get a COVID-19 vaccine, the situation for every person is different. It is best to discuss the risks and benefits of getting the COVID-19 vaccine with your cancer doctor, who can advise you.”
I have had my first Moderna shot one week ago. Is it okay for me to start taking prednisone and an antibiotic for my COPD flare up?
The vaccine should not affect the treatment for your flare up. The prednisone may diminish to some degree the response to your vaccination, but if you need it medically for your COPD flare up you should take your prednisone anyway and not worry about what effect this may have on responding to the vaccination. And it’s always a good idea to check with your healthcare provider for further clarification and specific instructions.
Does it matter which arm I get the shot in? Someone told me it needs to be your left arm.
Either arm works. People often choose the non-dominant arm just because if it gets sore it’s less of a nuisance.
If the second dose of maderna vaccine is the same as the first why is there more of a reaction the vaccininator told me to take the following day of work off because of adverse reactions. [armando fiorsani]
The reaction after the second dose may tend to be worse because the immune system is revved up from the first (identical) shot. If you have the option of waiting to decide about the day off, you may want to wait. Most people do not have bad reactions even after the second dose.
I recently learned about how using over-the-counter pain relievers or drinking alcohol prior to and following the Covid vaccine injection would impact the efficacy of the vaccine. Although the CDC has a sentence or two regarding use of OTC use prior to the vaccine, their FAQ response is too vague to be helpful. Please shed light on this issue. Also, I understand that OTC pain relievers can reduce the efficacy of ANY vaccine. A resource is provided here: “Don’t take a Tylenol or Advil before you get your COVID-19 vaccination and even if the shot hurts, you shouldn’t take one for a day or two after you get it, according to Dr. Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia and member of the FDA vaccine advisory board.”
We do not know exactly how much pain relievers or alcohol could reduce the effectiveness of your vaccine. However, it makes sense to avoid anything that could reduce your immune response, including inflammation, if possible.
Anti Inflammatory medicines (including ibuprofen-Motrin and others- and acetaminophen-Tylenol and others) should be avoided for 24 hrs before vaccination and for as long as possible (at least a few days) afterward. If pain is severe local measures such as intermittent ice in the first 24 hrs then heat after that can be helpful.
Excessive alcohol intake impairs the immune response. ”Excessive” is defined as “heavy drinking” (15 or more drinks/week for men and eight or more drinks/week for women) or “binge drinking” (5 or more drinks in a day for men or 4 or more for women). These should be avoided both before and after vaccination. Please note that if a regular, heavy drinker stops or reduces intake abruptly, withdrawal symptoms can result. Talk to your doctor if you are concerned about this. In short: avoid acetaminophen and ibuprofen, if possible–and for sure avoid excessive alcohol to help your body respond well to your Covid, or any other, vaccine.
Questions of Politics and Logistics:
Why are existing health systems like Florida HealthCare not being used to give the vaccine to their eligible patients? They are already routinely give flu shots, etc. and have a list of those who should get the vaccine. Thank you and the DOH who are doing a great job. [Carolyn Nicolin]
It’s hard to provide a simple answer to this question, but the real problem right now is just not enough doses of vaccine. If Florida HealthCare got some of our vaccine doses–in other words, if our county’s vaccine allotment remained the same but some went to Florida HealthCare, this would mean the Health Department would get less, so they would be giving some and we would be giving less, which would result in the same number of people in our county being vaccinated each week. The current arrangement is actually more efficient. Mass vaccination programs, which this is, are different than routine ongoing vaccination programs, and it’s hard for other health care organizations to “gear up” to vaccinate large groups of people. We at the Flagler County Health Department (actually my colleagues deserve the credit for this much more than me) are very experienced in this kind of thing, so it’s right up our alley. Between our staff and the large number of motivated and capable volunteers that have come forth to help us we are currently able to give 1000 doses of vaccine a day and we could double that in a week or two. At that higher rate (2000 vaccinations a day) we could get first shots into every resident of Flagler County in just 8 weeks, and by 16 weeks have everyone fully vaccinated with two doses. And that’s just us. It’s nice to have other places in the county, like Publix and soon additional pharmacies, stepping up to vaccinate people, because they offer convenience, but from our point of view at the Health Department we’d love it if as the vaccine allotments start increasing the state would send us the bulk of the vaccine designated for our county because we know we can get it into people’s arms very rapidly and efficiently–just ask anyone who’s been to our vaccination site. Since the start of this vaccination program we’ve gotten virtually 100% of the vaccine doses we’ve received into people within a week of receiving it. So come on, state of Florida, pour it on and give our county Health Department massive doses of vaccine! Which I think will actually start happening in March/April.
Could you please explain how a vaccine trial such as the Johnson and Johnson trial that has only 468 positive cases can show that these cases represent the true population of the US and are not just random results given that the study time to date is so short. With so few cases, and such a short time period – only 28 days post vaccination, how can it be concluded that the vaccine is the cause of only 28% of cases in the vaccinated group resulting in moderate to severe covid-19. In addition, many cases take time to progress. We hear over and over again that patients hospitalized don’t die until many weeks later. And some cases that seem mild at first progress after 10 or more days to severe. It seems like there is a rush to just put out any vaccine without actually getting the appropriate trial results.
Please let me clarify the details of this trial. It involved 44,325 subjects, approximately half of whom (i.e., about 22,000) received the vaccine. The trial was conducted in eight countries across three continents and included a diverse and broad population including 34% (N= 14,672) of participants over age 60. The study enrolled 44% (N=19,302) of participants in the United States, 41% (N=17,905) in Central and South America (Argentina, Brazil, Chile, Colombia, Mexico, Peru) and 15% (N=6,576) in South Africa. Forty-one percent of participants in the study had comorbidities associated with an increased risk for progression to severe COVID-19 (overall 41%), obesity (28.5%), type 2 diabetes (7.3%), hypertension (10.3%), HIV (2.8%); also other immunocompromised participants were in the study. The results of this study have not been published but they have been submitted to the FDA, so all the details are not available, but it was a very large trial involving a diverse group of subjects of different ages, in different locations around the world, and included patients with medical conditions putting them at increased risk of Covid. Because this was a prevention trial, they had to enroll so many subjects to get statistically significant data on the number of cases of Covid that were prevented. The 468 cases refers to the cases of Covid that occurred in subjects in this trial–a little more than 1% of the subjects enrolled in the trial–it is not referring to the number of subjects in the trial, which was almost 100 times larger. Most of these cases developed in the control group (about 3 times as many overall as in the vaccine group, hence the 66% effectiveness). The study design was quite good and very similar in design and size to the Moderna and Pfizer studies, and it generated safety data on over 22,000 subjects who received the vaccine. While it’s true the duration of the study was short, that was because the target efficacy numbers were met and they demonstrated robust statistical significance. There needs to be and will be ongoing surveillance data gathered on these subjects, which is why the application is for an EUA (Emergency Use Authorization) and not full FDA approval.
We also received the following: “Not a question….but a big Thank you to Dr Bickel and his staff for the great job they are doing…… it’s definitely appreciated…
You’re welcome!
Links to additional references (some of which Dr. Bickel referred to in preparing previous answers):
CDC Guidance on Allergic Reactions
CDC Fact Sheet on Covid Vaccines
New England Journal of Medicine–Answers to Frequently Asked Questions
Please be safe.
For a full, archived and indexed list of questions, go here.
![]()
Dr. Stephen Bickel, M.D.

Dr. Bickel, currently the medical director of the Flagler and Volusia County Health Departments, treats HIV and Hepatitis C patients at both departments, treats internal medicine patients at the Volusia Volunteers in Medicine free clinic, and is the medical consultant to the Community Care program at 9 Advent Health campuses in Florida.Dr. Bickel has a BA from Brown University, an MD from Rush Medical College, as well as MBA and MPH degrees from UCLA. He did residency training in internal medicine at Rush, public health/preventive medicine residency training at UCLA, as well as an endocrinology research fellowship at the University of Chicago. He is board certified in internal medicine and preventive medicine, as well as being a credentialed HIV specialist and a certified hypertension clinician.
He is very interested in how the social determinants of health impact our community and how we can address health disparities by improving our safety net. He has been on the Board of Directors of Flagler Cares since its inception.
![]()
Ask Dr. Bickel on FlaglerLive
Dr. Stephen Bickel, the medical director at the Flagler and Volusia County Health Departments, will be fielding your questions and regularly answering them on FlaglerLive. The "Ask the Doctor" column will be updated accordingly. Ask your question below. Your email will not be public. Dr. Bickel will strive to answer all questions. But similar questions will be grouped together, your questions may be edited for brevity and clarity, or withheld if deemed inappropriate or not relevant. Note the disclaimer.
Disclaimer: The content in FlaglerLive’s “Ask the Doctor” column is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. If you think you may have a medical emergency, call your doctor, go to the emergency department, or call 911 immediately. Reliance on any medical information provided by FlaglerLive.com or medical professionals presenting content for publication is solely at your own risk.





























Leave a Reply