Earlier this week the federal government clarified that insurers can’t charge people for anesthesia administered during a free colonoscopy to screen for colorectal cancer. That’s good news for consumers, some of whom have been charged hundreds of dollars for anesthesia after undergoing what they thought would be a free test. But the government guidance leaves important questions unanswered.
Under the health law, most health plans have to provide care that’s recommended by the U.S. Preventive Services Task Force without charging members anything out of pocket. The only exception is for plans that have grandfathered status under the law.
That task force, a nonpartisan group of medical experts, recommends that starting at age 50 people periodically receive either a colonoscopy, sigmoidoscopy or fecal occult blood test to screen for colorectal cancer.
Most people are anesthetized during a colonoscopy, in which a flexible tube with a camera at the end is inserted into the rectum and snaked through the large intestine to look for polyps and other abnormalities.
Although the health law made it clear that the colonoscopy itself must be free for patients, it didn’t spell out how anesthesia or other charges should be handled.
That lack of clarity allowed insurers to argue at first that if polyps were identified and removed during the colonoscopy, the procedure was no longer a screening test and patients could be billed. In 2013, regulators clarified that patients couldn’t be charged for polyps removed during a screening colonoscopy because it was an integral part of the procedure.
With this week’s guidance, the government has made it clear that consumers don’t have to pick up the tab for anesthesia during a colonoscopy either.
But other questions remain. Consumers may still find themselves on the hook for facility or pathology charges related to a screening colonoscopy, according to an email from Anna Howard, a policy principal at the American Cancer Society Cancer Action Network, and Mary Doroshenk, director of the National Colorectal Cancer Roundtable.
In addition, cost sharing rules are unclear for consumers who get a positive result on a blood stool test and need to follow up with a colonoscopy. The federal government hasn’t clarified whether that procedure is considered part of the free screening process or whether insurers can charge for it as a diagnostic procedure, Howard and Doroshenk say.
In a 2012 study, researchers found that four insurers imposed patient cost sharing for colonoscopies after a positive blood stool test and three did not.
As for consumers who paid for anesthesia and now learn that they shouldn’t have been charged, it’s unclear if they can get their money back.
“Our expectation is that those who have received a bill for anesthesia this plan year may be able to appeal, but not for previous years,” Howard and Doroshenk said.
The Department of Health and Human Services didn’t respond to a request for clarification.
–Michelle Andrews, Kaiser Health News





























Outsider says
I wonder when liberals will stop believing in the fantasy that anything can be “free.”
a tiny manatee says
With all of the conservative assholes out there, you would think they would be behind this 100%.
FFS says
LOL – Thanks for the laugh, a tiny manatee. That was a brilliant response!
Groot says
If a person has ever had a positive colonoscopy or a polyp removed, the insurers do not have to pay for it and they do not. It goes on the deductible and the co-pay. Thank you ACA.
FFS says
Good to know. I’m in my mid 30’s and have to go back every 2 years due to a cancerous spot that I had to have removed already. Mine was found before the ACA kicked in, so I wondered what would happen with my follow ups. Thanks for the info Groot.
Groot says
If you have had a positive test in the past or a spot or a polyp removed, your ACA compliant plan will cover it but it is then deemed to be a diagnostic test and not a preventive test. It all falls on your deductible and your co-pay. My retirement system and my health insurance provider just sent us all a letter about this and clarified it. While it is a covered procedure, it is not free if you have ever in your life had a positive test, a polyp or spot removed, the deductible and the co-pay apply. It is considered diagnostic and it is not a free of charge ACA preventive procedure.
Coleen says
Holy Crap…isn’t anything sacred anymore ?
Sherry E says
The colonoscopy is not “FREE” the ACA is simply requiring that test be “covered completely” by your insurance. Folks, this is a GOOD thing! An expensive, possibly life saving, test that the ACA is requiring be covered without your “out of pocket” money. This is yet another example of insurance companies looking for loopholes in the federal law so that they can continue to charge you for services they break out into different pieces. . . and different circumstances.
Anonymous says
Go ahead and blame Obamacare, you Tea party sheepies. It’s the insurance companies who, with all the doctors and nurse’s that they have on their case review staffs, can’t seem to have figured out that a Colonoscopy requires anesthesia and pathology and a clean adequate place for the procedure to take place. Of course, they know this–It isn’t rocket science! The insurance companies are trying as hard and in as many circumstances as their corporate minds can figure out how to avoid paying for necessary services by saying “We will disallow even the most obvious and sensible of services unless the government (big baddie that it is) spells out every single little thing, to the remotest detai,l what we are absolutely forced by written law to cover. Otherwise, we have no moral, ethical or medical obligation to our consumers at all.
Sherry E says
@Groot et al. Suggest you appeal your claim as some insurance companies have backed down on those denials of claim payments. This from Kaiser. . . note the new codes that should be used:
“Recently there have been efforts by the American Medical Association (AMA) to modify the Current Procedural Terminology (CPT) coding system to clearly designate preventive services that should be covered without cost-sharing. In direct response to the new ACA requirement, CPT modifier 33 was created to allow providers to identify to insurance payers and providers that the service was preventive under applicable laws, and that patient cost-sharing does not apply. The AMA writes that the modifier “may be used when a service was initiated as a preventive service, which then resulted in a conversion to a therapeutic service. The most notable example of this is screening colonoscopy (code 45378), which results in a polypectomy (code 45383).”14
Insurers vary, however, in the coding methods they use and in what codes their claims payment systems can accommodate. Some insurers have encouraged providers to use CPT modifier 33, but another medical director cautioned that claims systems vary widely and not all insurers’ systems are designed to use this modifier. “
YankeeExPat says
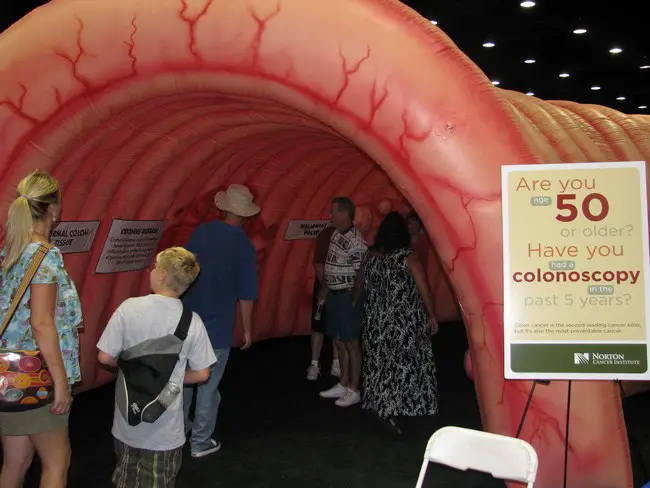
O.K. The Joke is on Me. I thought the Picture accompanying this article was showing the entrance to the State House in Tallahassee, my bad.
Sherry E says
LOL! YankeeExPat. . . my laugh of the morning. . . Thanks! LOL! You are just so Right On! LOL!