In this latest installment of FlaglerLive’s “Ask the Doctor” column by Dr. Stephen Bickel, the medical director at the Flagler and Volusia Counties Health Departments, the doctor takes on recurring questions about the covid vaccine’s safety, its effectiveness against new variants of the virus, and many other questions. Dr. Bickel relies substantially on the New England Journal of Medicine for this latest installment.
Dr. Bickel, featured almost weekly on WNZF’s Free For All Friday program since last March to update the community on the coronavirus pandemic and answer questions, will be doing so on a rolling basis here. The questions don’t have to be limited to the pandemic.
You are invited to submit your questions using the form below. The entire list of questions will be archived, indexed and linked to their answers on a separate page, here.
The “Ask the Doctor” column is a semi-regular feature of FlaglerLive. “Please feel free to ask any medical question you want,” the doctor says, “and I will do my best to answer it. In preparing my answer to your question, I may consult with some of my medical specialist colleagues or review the medical literature in order to come up with the best possible answer.
“Please limit your questions to general medical advice—I can’t give you specific medical advice since I don’t know your individual medical history. The emphasis of this column will be to provide information based on current scientific evidence while keeping speculation and politics to a minimum. If I don’t know something or the medical literature really doesn’t have much to say on a particular topic, I will tell you that.”
Previous installments of the “Ask the Doctor” column are available here, here, here and here.
![]()
By Stephen R. Bickel, M.D.
What do we know about the vaccines’ short-term safety?
Overall, both mRNA vaccines are quite safe. Indeed, in the first published safety review of 13.8 million doses given in the first month after the vaccines’ release, no serious or unexpected adverse events were noted. This is especially reassuring since the first wave of vaccinations went to many frail, older people who are more at risk for side effects. But no vaccine (actually, nothing in medicine) is 100% safe, and the safety of Covid-19 vaccines will be in the spotlight for some time — these are new vaccines for a new disease. Rare events will appear in the news, amplifying attention and worry disproportionate to the actual risk.
These first two vaccines are classified as “reactogenic” — meaning they will cause some side effects in most people who receive them, reflective of the brisk immune response they generate. The most common side effect is pain at the injection site, especially in the 12 to 24 hours after administration. Fatigue and headache are other relatively common side effects; high fevers are less common. These side effects generally resolve within a couple of days and are responsive to acetaminophen or an antiinflammatory drug such as ibuprofen. In general, side effects are more common in younger vaccine recipients than in older ones, with the second shot inducing more side effects than the first.
Some people receiving the Moderna vaccine experience redness, warmth, and/or itching around the injected site—this is usually a delayed reaction that typically occurs 5 to 14 days after the shot. In the clinical trials, Bell’s palsy was reported more frequently in vaccine recipients than in controls, but there was not a sufficiently large number of cases to conclude that this was beyond what would naturally be observed in populations of this size by chance. There were no cases of Guillain–Barré syndrome or transverse myelitis.
Although hypersensitivity occurred equally in the placebo and vaccine groups in both trials, after distribution of the vaccines in the United Kingdom and the United States, reports emerged of severe allergic reactions in some individuals, shortly after being vaccinated. The current leading suspect in causing these reactions is polyethylene glycol, a compound present in both vaccines. Because of these rare events, administration of the vaccines includes a period of 15 minutes of observation after vaccination — 30 minutes for those with a history of severe allergic reactions of any sort. These allergic reactions are uncommon — the current estimate is that anaphylaxis will occur rarely, approximately once out of every 200,000 (or more) people vaccinated. Although these rates of severe allergic reactions are higher than those with other vaccines, they are substantially lower than the rate reported with penicillin, which is estimated to be 1 in 10,000.
Since the first phase of people vaccinated with these vaccines included older people — many of them with other medical problems, or in nursing homes, or both — some vaccine recipients have died after receiving their immunizations. Through February 21, 2021, more than 63 million doses have been administered, with 1099 reports of death. Each of these cases is reviewed by CDC and FDA physicians, including medical records, death certificates, and (when available) autopsy reports. Thus far there has been no identified link with vaccination.
What do we know about the vaccines’ long-term safety?
Because of the fast pace of vaccine development we have had only months, not years, of follow-up. (Both mRNA clinical trials started in the summer of 2020.) But with other immunizations, severe reactions typically occur within days or weeks after administration.
Further safety data on both vaccines will be reported to the VAERS (Vaccine Adverse Event Reporting System.This program is an existing national early warning system that was set up to detect possible safety problems in any licensed vaccine and has been in operation since 1990. In addition, the CDC has its own smartphone-based tool, which uses texting and a Web-based survey to collect information right after patients receive their Covid-19 vaccine.
Will the vaccines work against the emerging strains of SARS-CoV-2?
Currently there is limited information on how effective the mRNA vaccines will be against emerging strains of SARS-CoV-2. Both the Pfizer and Moderna clinical trials preceded the identification of the major variants present now in multiple countries around the world. Studies suggest that the vaccines might be more protective against some of the variants than others, so no broad generalization about vaccine activity against variants is possible. An important limitation of these studies is that protection afforded by vaccination is more complex than simply measuring antibody responses.
From a practical perspective, the discovery of these variants does not change the basic recommendations for vaccination. Specifically, right now it is not recommended that people wait for a new or changed vaccine in the hope that it will be more effective against emerging SARS-CoV-2 variants, though both Pfizer and Moderna are developing modifications to their existing vaccines designed specifically for broader activity against emerging strains.
Do the vaccines prevent transmission of the virus to others?
There is growing evidence that mRNA vaccine recipients are less likely to transmit infection to others. In a large observational study conducted in Israel, those who had been vaccinated had a 90% reduction in the risk of asymptomatic infection. Furthermore, among those who do get infected after vaccination, it appears that viral loads are lower than in non-vaccinated people who get infected. Lower viral loads most likely lead to reduced risk of transmission. These data serve as a reminder that many vaccines in wide use today powerfully protect against both disease and transmission — so much so that infection control is one of the main motivators behind vaccination campaigns.
Please note, however, that while the vaccines do reduce the risk of transmission, we cannot say they eliminate it — the protective effect will never be 100%. As a result, until case numbers are down and a higher proportion of the population has received their vaccines, we need to continue to employ other important measures to prevent the spread of Covid-19 such as mask wearing in public, social distancing, and avoiding crowded indoor settings.
Should patients who have recovered from Covid-19 receive the vaccine?
Yes, they should receive the vaccine. Some of the people who participated in the clinical trials had evidence of prior SARS-CoV-2 infection (based on a positive antibody test), and the vaccines were safe and effective in this group. Because re-infection after recovery from Covid-19 is rare in the first 90 days, some people may wish to defer immunization for this long — however, if they wish to be immunized sooner, there is no contraindication.
Patients who were treated with monoclonal antibodies or convalescent plasma should wait 90 days, however, because these treatments could theoretically reduce the efficacy of the vaccines. The reason 90 days was selected was because this duration factors in both the known half-life of these therapies and the low likelihood that someone with Covid-19 will experience reinfection in this time period.
Since publication of the clinical trials, researchers have reported that people with prior Covid-19 who received immunization with the mRNA vaccines had more pronounced antibody responses (and more systemic side effects) after their first vaccine dose than those who were seronegative. As a result, there has been some debate about whether a second dose of the vaccine is necessary for this group, but for now, a second vaccine dose is still recommended.
Are there contraindications to any of the vaccines?
The only absolute contraindication to these vaccines is known hypersensitivity to the vaccine components. Specific CDC recommendations regarding contraindications list the following:
Severe allergic reaction (e.g., anaphylaxis) after a previous dose of an mRNA Covid-19 vaccine or any of its components
Immediate allergic reaction of any severity to a previous dose of an mRNA Covid-19 vaccine or any of its components (including polyethylene glycol [PEG])
Note that anaphylaxis in reaction to any other vaccine or injectable therapy is not a contraindication to these Covid-19 vaccines, but persons with this history should be observed for at least 30 minutes after they receive their dose.
If a person experiences a severe reaction (in particular anaphylaxis) to the first shot, the person should not receive the second. People who experience severe pain will need to make an individual decision about whether to proceed with the second shot — it is not contraindicated, but side effects tend to be worse with the second dose. One potential strategy is to administer acetaminophen or ibuprofen as soon as the pain starts after the second dose. The CDC does not recommend pre-vaccine administration of these drugs, since theoretically they could blunt the vaccine-induced antibody response, and they are often unnecessary.
Can a patient with a history of an allergic reaction receive the vaccine?
Someone with a history of allergies can definitely receive the vaccine — it doesn’t matter whether it’s an allergy to other vaccines or medications or to bee stings or food or pollen. However, people with these histories should be observed for 30 minutes after receiving the vaccine, rather than the usual 15 minutes.
As has been widely reported, there have been rare cases of severe allergic reactions to the first dose. When this occurs, the second dose should not be given. It is not currently known whether these people would have allergic reactions to other experimental Covid-19 vaccines that do not use the mRNA mechanism of action.
Should pregnant or breastfeeding individuals receive the vaccine?
Although pregnant and breastfeeding individuals were not enrolled in the original Covid-19 vaccine trials and as a result there are limited data about safety in these groups, the CDC advises that those who are pregnant or lactating may get vaccinated if they so choose. Importantly, there is no theoretical reason why mRNA vaccines would be harmful to the mother during pregnancy, to a developing fetus, or to a breastfeeding infant.
Observational studies have shown that pregnancy is a risk factor for severe illness due to Covid-19, much as it is for influenza. On the basis of this information and their likelihood of Covid-19 exposure, along with information about the limited safety data available to date, pregnant individuals can make an educated decision about whether to accept the vaccine.
Should acetaminophen or nonsteroidal antiinflammatory drugs be taken prior to vaccination to prevent post-vaccination symptoms?
Although these drugs could decrease subjective side effects, theoretically they could also blunt the immune response and make the vaccines less effective — hence they are not recommended before vaccination. They are useful, however, in diminishing side effects once they occur. Acetaminophen is preferred for pregnant individuals.
Links to additional references:
CDC Guidance on Allergic Reactions
CDC Fact Sheet on Covid Vaccines
New England Journal of Medicine–Answers to Frequently Asked Questions
Please be safe.
For a full, archived and indexed list of questions, go here.
![]()
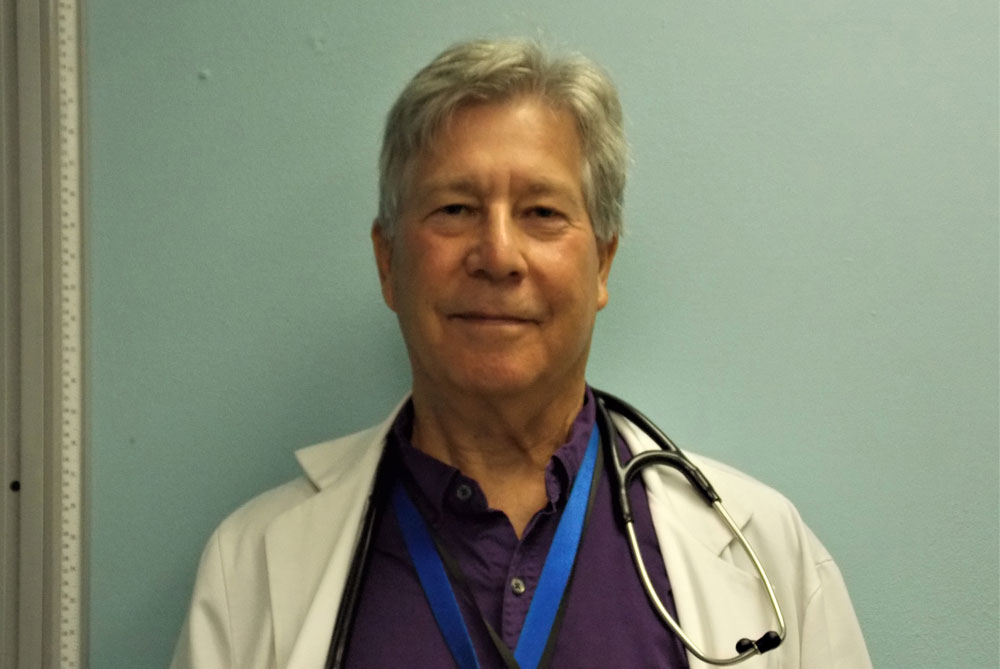
Dr. Stephen Bickel, M.D.

Dr. Bickel, currently the medical director of the Flagler and Volusia County Health Departments, treats HIV and Hepatitis C patients at both departments, treats internal medicine patients at the Volusia Volunteers in Medicine free clinic, and is the medical consultant to the Community Care program at 9 Advent Health campuses in Florida.Dr. Bickel has a BA from Brown University, an MD from Rush Medical College, as well as MBA and MPH degrees from UCLA. He did residency training in internal medicine at Rush, public health/preventive medicine residency training at UCLA, as well as an endocrinology research fellowship at the University of Chicago. He is board certified in internal medicine and preventive medicine, as well as being a credentialed HIV specialist and a certified hypertension clinician.
He is very interested in how the social determinants of health impact our community and how we can address health disparities by improving our safety net. He has been on the Board of Directors of Flagler Cares since its inception.
![]()
Ask Dr. Bickel on FlaglerLive
Dr. Stephen Bickel, the medical director at the Flagler and Volusia County Health Departments, will be fielding your questions and regularly answering them on FlaglerLive. The "Ask the Doctor" column will be updated accordingly. Ask your question below. Your email will not be public. Dr. Bickel will strive to answer all questions. But similar questions will be grouped together, your questions may be edited for brevity and clarity, or withheld if deemed inappropriate or not relevant. Note the disclaimer.
Disclaimer: The content in FlaglerLive’s “Ask the Doctor” column is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. If you think you may have a medical emergency, call your doctor, go to the emergency department, or call 911 immediately. Reliance on any medical information provided by FlaglerLive.com or medical professionals presenting content for publication is solely at your own risk.





























tulip says
Thank you Dr. Bickel for being such a big help to us with our questions and concerns. It’s been very reassuring and plain simple talk and easy explanations.
Lynne says
There are currently 55 events in the VAERS CDC Wonder system of suspected Guillain-Barre syndrome and transverse myelitis related to Covid-19 vaccines.
https://wonder.cdc.gov/controller/datarequest/D8;jsessionid=1E1781DC01E2A580141DE44B1C5E
Concerned Citizen says
Gotta love how they prioritized lives.
As an essential worker at 50 something years old I had to go to work every day. Lockdown or not. And still do. And now here I sit while others more important than I are fully vaccinated.
What this pandemic has shown is we are all expendable.